What Is Antimicrobial Resistance?
5. Overview
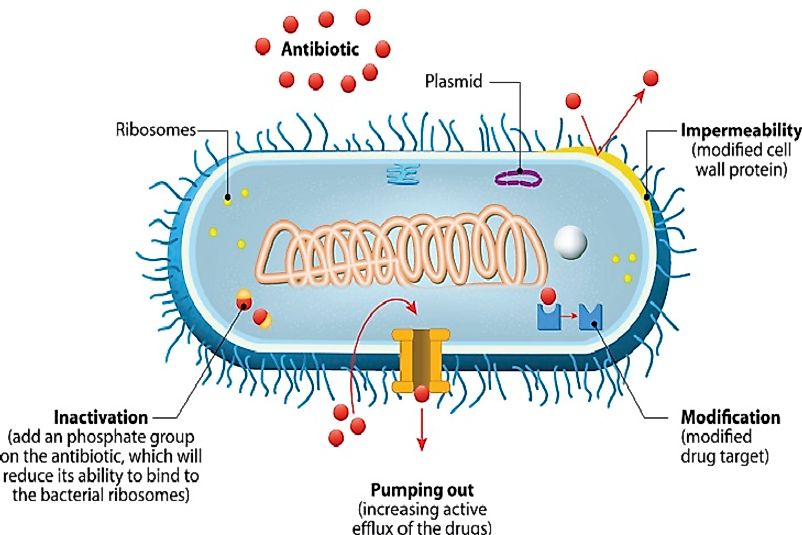
Antimicrobial resistance refers to the resistance of a microbial organism to a drug or an agent that was previously effective in eliminating the organism or checking its growth and multiplication. Drug resistant strains generally evolve over a period of time in nature. However, improper and unscientific use of antimicrobial agents speeds up this process, generating strains of microbes that cannot be controlled by the antimicrobial agents, triggering wide scale spread of the drug resistant infectious disease.
4. Antimicrobial versus Antibiotic Resistance
The word antimicrobial has been derived from the Greek words anti (against), mikros (little) and bios (life) and refers to all agents that are able to kill (microbicidal) or retard the growth of (biostatic) such microorganisms as bacteria, fungi and protozoans. However, the word antimicrobial is not synonymous to the word antibiotic as the latter, derived from the Greek word, anti (against) and biotikos (concerning life), refers to only those antimicrobial agents that are produced by microorganisms themselves and act against other microbes. The antibiotics are thus purely extracted from microorganisms unlike many other antimicrobial agents which are produced by synthetic means or extracted from plants or animals.
3. Factors Causing Antimicrobial Resistance
The widespread use of antimicrobial agents without strictly adhering to the scientific principles guiding their use, has led to the development of microbial strains resistant to the antibiotics. The increasing global availability of the antimicrobial drugs and the uncontrolled use of the antimicrobial agents in low or middle income countries where laws to restrict sale of non-prescribed antimicrobial agents do not exist, are the primary reasons behind the development of antimicrobial resistance. Antimicrobial resistance also arise when doctors prescribe antimicrobial agents upon patient insistence. Over half of the cases of antimicrobial prescribed are unnecessary and one-third of the people bear the common misconception that antibiotics are needed during the viral infection of common cold. The tendency to miss doses or use antimicrobial agents over a long term with gap periods also tends to encourage the growth of antimicrobial resistant organisms. Use of antibiotics as livestock feed has also sped up the evolution and growth of antibiotic resistant. The release of large volumes of antimicrobial agents into water bodies without proper waste water treatment by pharmaceutical companies contributes to antimicrobial resistance.
2. Who's Most At Risk?
Antimicrobial resistance is a cause of great health and safety concern. With microbes being able to withstand the effects of drugs, more and more diseases will become incurable. Diseases like pneumonia and tuberculosis, which have been brought under control by the use of antimicrobial medications, will again start claiming lives. The hard work of previous scientific research will all fail and there will be an increasing need of rapid development of new and more powerful drugs targeting the drug resistant microbes. All this will result in heavy economic losses of the patients and their families as well as the healthcare systems of the world. More and more people will become the prey of infectious diseases and those at higher risk of exposure will suffer even more. Children and elderly people as well as those with diseases resulting in a weakened immune system will be easily infected by the drug resistant microbes. People living in crowded, unhygienic conditions, as well as healthcare workers, veterinarians, farmers, and others who are frequently exposed to infectious agents, will also be more likely to succumb to these drug-resistant infections.
1. What Can Be Done?
Antimicrobial resistance can be prevented only by spreading widespread public awareness. People need to understand why responsible use of antimicrobial agents is important to save lives in the long term. Only antimicrobial agents prescribed by a registered medical practitioner must be consumed and the entire prescribed dose must be finished to ensure that no bacteria survives to emerge as antimicrobial resistant. Antimicrobial agents should be avoided during viral infections unless prescribed by doctors if they deem it necessary. Healthcare professionals play the most important role to guide and illuminate patients about the phenomenon of antimicrobial resistance. They also must prescribe medications in the correct dose and for the correct duration. There is also a great need to stop the over-the-counter sale of antimicrobial agents in some countries which often leads to the improper use of these drugs.